9.8 AGE-RELATED DISEASES OF BONE: OSTEOPOROSIS
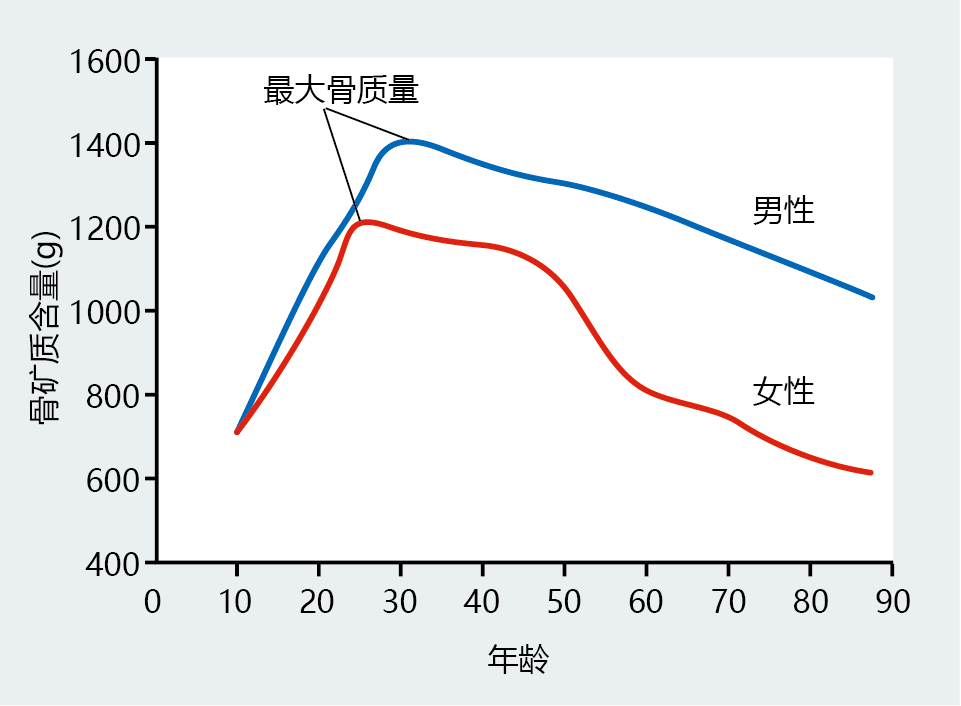
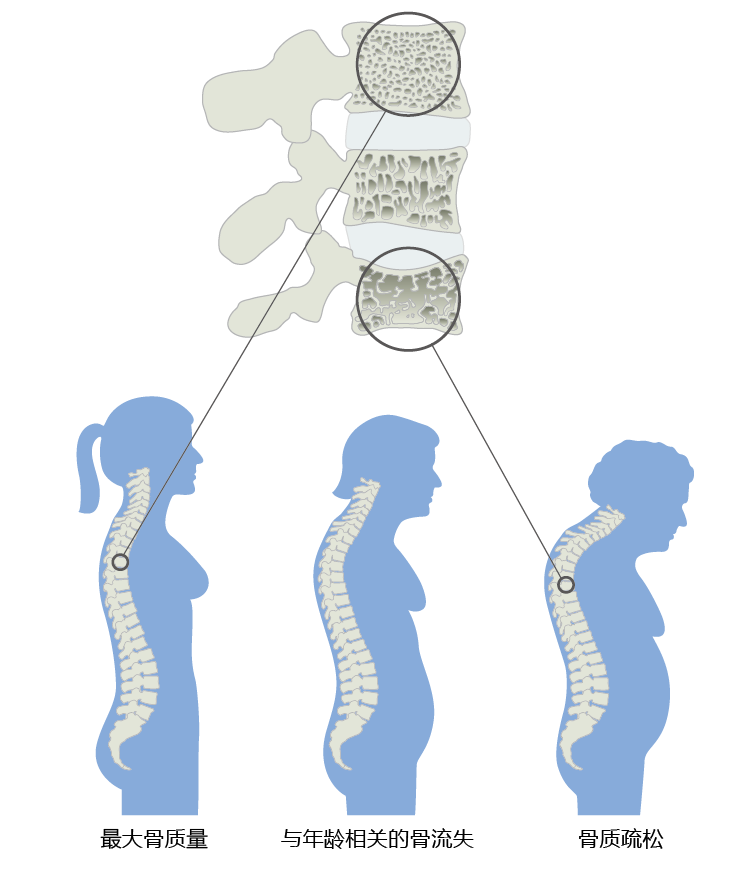
The average height of women and men decreases after the age of 50. The loss in height reflects a slight compression of the vertebrae caused by declining bone mineral content after peak bone mass has been achieved (Figures 9.37 and 9.38). The accelerated loss of bone mass in women after menopause (~50+) reflects declining estrogen levels and places women at a significantly greater risk of developing osteoporosis, a bone disease characterized by low bone mass and strength, which leads to an increased risk of fracture. In fact, 80% of all cases of osteoporosis occur in women. Although men also experience age-related bone loss, they do not, in general, develop primary osteoporosis (that caused only by age-related bone loss) until the tenth or eleventh decade of life. Younger men can, however, develop secondary osteoporosis, caused by such things as medication, cancer, and kidney disease.
Figure 9.37 Total body bone mineral content (BMC) in males and females throughout the life span. Females tend to achieve peak bone mass at a younger age than males. The slow rate of BMC loss after peak bone mass is approximately the same for men and women, until menopause (50+ years of age). Note the accelerated rate of decline in BMC in women after the age of 50. (Data from World Health Organization, Prevention and Management of Osteoporosis, WHO Technical Report Series 921, Geneva: World Health Organization, 2003.)
Figure 9.38 Progression of vertebral bone loss in women, causing a decrease in height. The age-related loss of bone calcium results in compression of the vertebral body, which causes the entire spinal column to shrink, decreasing height. Excess bone loss in the vertebrae results in osteoporosis and a curvature of the spine sometimes known as a dowager's hump.
The increased rate of bone loss in women after menopause provides us with a rare opportunity to explore, in humans, the relationship between age-related loss and reproductive life span. In this section, we discuss the development of primary osteoporosis in women from a perspective of reproductive senescence, exploring how normal bone mineral loss transitions into osteoporosis in postmenopausal women.
9.8.1 An increased rate of bone mineral loss at menopause can lead to osteoporosis
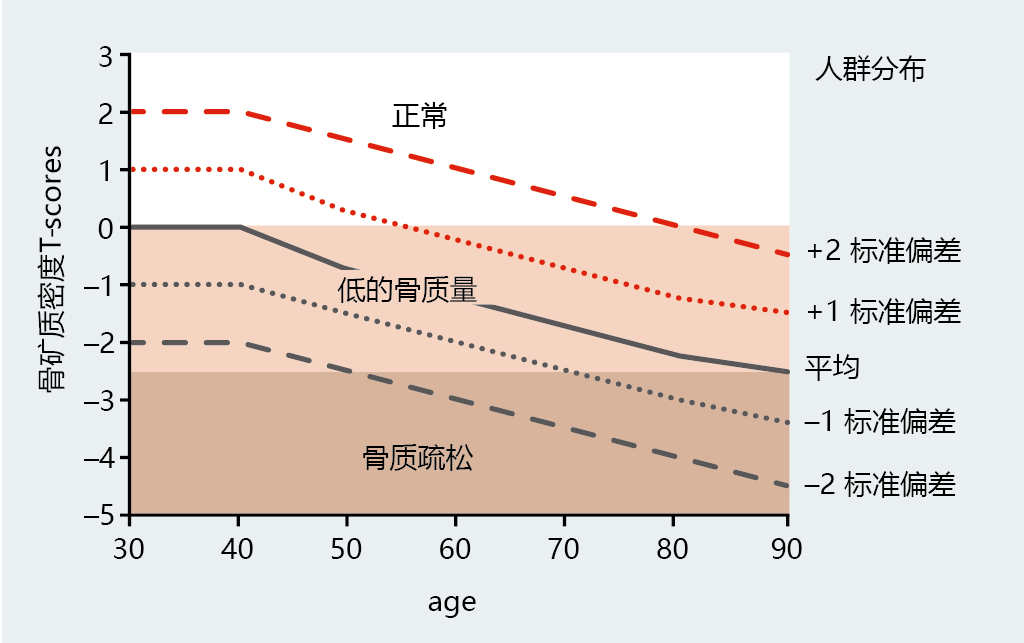
The increased rate at which women lose bone mineral after menopause places them at a significant risk for developing osteoporosis. The World Health Organization has suggested a diagnostic classification of osteoporosis as a bone mineral density (BMD) (measured in grams of mineral/cm 2) at the hip or spine of ≤ 2.5 standard deviations (SDs) below the young population's normal mean (Figure 9.39). For ease of comparison across age groups, the WHO refers to the statistical distribution (mean ± SD) of the young normal population as a T-score. T-scores of ≥ −1 are considered normal and pose no additional risk for developing osteoporosis. Values between −1 and −2.5 indicate a low bone mass, clinically known as osteopenia, and an increased risk of developing osteoporosis. Interestingly, the normal BMD for women over the age of 60 declines to the low bone mass range, suggesting that age is a major risk factor for osteoporosis. Although the WHO distribution indicates that women 90+ years of age normally have osteoporosis, limited data for this population make these values unreliable.
Figure 9.39 The WHO's diagnostic criteria for osteoporosis in women. Osteoporosis is defined as a bone mineral density (BMD, g/cm 2) at the hip or spine of ≤ 2.5 standard deviations below the young normal mean reference (premenopausal, 30 –40 years of age). This value is presented as a T -score (left y -axis). The graph lines represent the population distribution of BMD for women at various ages (right y -axis).
9.8.2 环境因子influence the risk of developing osteoporosis
More than 100 years ago, Julius Wolff, a German surgeon, found that bones become thicker—that is, BMD increases—when placed under increased load. His observation led to the development of Wolff's law: bones grow in direct proportion to the load placed upon them. For example, the BMD of the radius (the large bone in the forearm) in the dominant arm of professional tennis players is consistently greater than that of the radius in the nondominant arm. Intensive load-bearing exercise increases BMD, and disuse of bone leads to a decrease in BMD. This effect has classically been observed in patients undergoing long periods of bed rest and in astronauts after spending time free from Earth's gravitational force. Thus, lack of physical activity can increase the risk of developing osteoporosis. However, the effectiveness of moderate exercise programs in increasing BMD remains uncertain.
The greatest gains in BMD among postmenopausal women who start a light to moderate weight-bearing exercise program occur in previously sedentary individuals. Only small gains in BMD are observed in women who exercise regularly.
Recall that estrogen modifies the full effect of PTH-induced bone resorption by stimulating osteoclasts' deposition of bone mineral and inhibiting resorption by osteoblast. When estrogen concentrations decline during and after menopause, the bone dumps greater amounts of Ca2+ into the serum, and, in turn, excretion of calcium in the urine increases in order to maintain serum Ca2+ in the 9–10 mg/dl range. The increase in urinary calcium can often be greater than dietary intake, a phenomenon known as negative Ca2+ balance. Increasing the dietary intake of Ca2+ often eliminates a negative Ca2+ balance in young, premenopausal women and helps to maintain bone mass. However, similar treatment in postmenopausal women has not been as effective in maintaining premenopausal levels of BMD. The National Academy of Sciences has set the recommendation for daily Ca2+ intake by postmenopausal women at 1200 mg/day. This amount has proved effective in combination with medication and increased physical activity for previously sedentary individuals.
Intestinal absorption of dietary Ca2+ requires vitamin D. Older individuals' declining dietary intake and limited exposure to ultraviolet light (skin synthesizes vitamin D on exposure to UV light) may decrease the amount of vitamin D available for appropriate Ca2+ absorption. Increasing the dietary intake of vitamin D has been shown to increase the absorption of Ca2+ in postmenopausal women. However, the vitamin D-induced increase in Ca2+ absorption has not been shown to increase BMD in non-osteoporotic, postmenopausal women. Nonetheless, because the data are conflicting, clinicians often recommend increasing the intake of vitamin D along with Ca2+ as a precautionary measure.
Women's bone mineral content reaches its peak at the age of ~25 years. Thereafter, bone mineral content slowly declines until menopause, when the rate of mineral loss sharply increases. The rate of loss in both the pre- and postmenopausal age groups does not depend on the amount of bone mineral at the time of peak bone mass. This phenomenon is shown nicely in Figure 9.39. Women with a peak bone mineral content ≥1 SD above the mean have the same rate of loss as do other groups. However, these women do not reach the osteoporosis threshold during their life span. In fact, women with exceptionally dense bones (+2 SD above mean) may not even reach the low bone mass threshold. In other words, the more bone mineral you have at peak bone mass, the more bone mineral you will have later in life. Attaining one's genetic limit for bone mineral content at the time of peak bone mass has been widely accepted as a primary prevention strategy for reducing one's risk of developing osteoporosis.
Recommendations aimed at helping young women achieve their maximal peak bone mass have, for the most part, focused on improving dietary Ca2+ and vitamin D intake, as well as increasing weight-bearing exercise. The chances of achieving maximal peak bone mass are greatly enhanced if young women follow the recommendations suggested by the Food and Nutrition Board of the National Academy of Sciences. That is, girls under the age of 18 years should consume at least 1300 mg of Ca2+ and 5 mg of vitamin D per day. In addition, high dietary intake of specific vitamins and minerals should be accompanied by increased weight-bearing physical activity.
9.8.3 Drug therapies can slow bone loss in postmenopausal women
Focusing on preventive measures for young women does not imply that older women will not benefit from exercise or dietary improvement. However, increasing weight-bearing activity, dietary Ca2+, and/or vitamin D levels only slows, and does not prevent, bone loss in preor postmenopausal women. Stopping the loss and increasing bone mineral content after peak bone mass or menopause can be achieved only through pharmacotherapy. However, increased physical activity along with increased Ca2+ and vitamin D intake in combination with pharmacotherapy significantly enhances bone mass and reduces the rate of fracture compared with drugs alone. Here we look at three of the more common types of drugs used to increase bone mass in postmenopausal women: estrogen, specific estrogen receptor modulators (SERMs), and bisphosphonates.
Since estrogen stimulates osteoblast activity (bone formation) and inhibits osteoclast activity (bone resorption), it should not be surprising that estrogen replacement (also known as hormone replacement therapy, or HRT) has found significant acceptance as a therapeutic agent in preventing postmenopausal bone loss. Virtually every study investigating the use of HRT as a treatment for osteoporosis has found increased bone mass and/or a decreased rate of fracture. Unfortunately, recent evidence reveals that the use of HRT at levels needed to increase bone mass also increases the risk of breast cancer. The increased risk of breast cancer has significantly reduced the use of estrogen as the first line of defense against excessive bone loss and osteoporosis. Estrogen replacement for prevention or treatment of osteoporosis is now relegated to use when other treatments fail or when the risk of health problems due to fracture outweighs the risk of cancer.
SERMs are a class of compounds that have selective actions, depending on which estrogen receptor, α or β, they bind to. For example, tamoxifen (Nolvadex) increases bone density by stimulating osteoblast activity but inhibits the growth of breast cancer tissue by blocking the binding of endogenous estrogen to its receptor. Tamoxifen's severe side effects and relatively weak action on bone have led to its use primarily as a cancer treatment. Raloxifene (Evista ®) was developed specifically to treat osteoporosis, although it has recently been approved for treat ing women at high risk for breast cancer. Clinical trials have found that raloxifene is more effective than tamoxifen at reducing hip and vertebral factures, but is less effective than estrogen. Raloxifene does not produce the severe side effects observed with tamoxifen—namely, uterine inflammatory diseases and an increased risk of uterine cancer.
Bisphosphonates are a group of compounds that induce apoptosis in osteoclasts and thus inhibit bone resorption. Bisphosphonates disrupt normal ATP synthesis by creating a carbon-phosphate bond in place of the normal oxygen-phosphate bond. Because ATPase can break only the oxygen-phosphate bond, the carbon-phosphate ATP builds to toxic levels in the osteoclast and induces apoptosis. The three FDA approved bisphosphonates are alendronate (Fosamax ®), ibandronate (Boniva ®), and risedronate (Actonel ®). All three are equally effective at slowing the rate of bone mineral loss in postmenopausal women and decreasing the risk of hip and vertebral fractures. There remains some controversy as to whether bisphosphonates help increase bone mass or simply stop the loss of bone mineral content.
ESSENTIAL CONCEPTS
- The human nervous system is composed of the central nervous system (CNS), consisting of the brain and spinal cord, and the peripheral nervous system (PNS), consisting of all other nerves outside the CNS.
- Neural cells (neurons) are made up of three basic components: dendrites, the cell body, and the axon.
- Neurotransmission is propagated by establishment of an action potential, a brief depolarization of a small section of the nerve cell membrane.
- Neurotransmitters relay electrical messages from one neuron to another across synapses. A synapse is made up of the axon terminal of the presynaptic neuron, the dendrite of the postsynaptic neuron, and the synaptic cleft.
- Age-related changes in the human brain are minor and do not seem to significantly affect brain function.
- Accumulation of two 蛋白质 aggregates, amyloid plaques and neurofibrillary tangles, in the human brain appears to be a normal age-related phenomenon.
- The cause of Alzheimer's disease is unknown, but individuals with Alzheimer's are found to have high concentrations of amyloid plaques and neurofibrillary tangles.
- There are three general forms of Alzheimer's disease: early onset, late-onset, and familial. Early-onset and familial Alzheimer's are genetic in origin, whereas the late-onset form does not seem to be inherited.
- Parkinson's disease results from the loss of dopamine-producing neurons in the substantia nigra region of the basal ganglia.
- The heart consists of two separate pumps: the right side delivers oxygen-poor blood to the pulmonary system (lungs); the left side supplies oxygen-rich blood to the body.
- The muscle of the heart and arteries is excitable tissue. That is, the muscle generates action potentials in response to neural and hormonal stimulation.
- Cardiac output is determined by the amount of blood returned to the heart. Stretching of the heart muscle in response to venous return determines the force necessary to eject blood from the ventricles.
- Arterial plaques, accumulations of cholesterol-filled fatty deposits in the arteries, are present in 100% of the aged population. Excess accumulation of arterial plaques results in the disease atherosclerosis.
- Age, smoking, hypertension, and hyperlipidemia are the major risk factors for coronary artery disease.
- More than 50% of individuals 65 years and older have hypertension (high blood pressure), defined as a consistent systolic blood pressure of ≥140 mm Hg or diastolic pressure of ≥90 mm Hg.
- Heart failure can be defined as the inability of the myocardium to generate the contractile force needed to eject the blood volume required for the oxygen demands of the body—that is, an abnormal decrease in cardiac output.
- Blood 葡萄糖 is maintained within a narrow range of 90–120 mg/dl by the competitive action of two hormones produced by the endocrine cells of the pancreas: insulin and glucagon. This level of blood 葡萄糖 must be maintained because the brain uses only blood 葡萄糖 for its energy needs.
- Insulin facilitates the uptake of 葡萄糖 into cells by initiating an intracellular signaling cascade. Insulin can also regulate the metabolism of fats and 蛋白质.
- Insulin resistance is the inability of insulin to effectively stimulate 葡萄糖 uptake into cells. It is a major risk factor for type 2 diabetes.
- The major outcome of type 2 diabetes is damage to microvascular blood flow. Without proper blood flow, tissue can be damaged, leading to tissue death.
- Estimates indicate that more than 80% of new cases of type 2 diabetes are caused by obesity. Maintaining a healthy weight is considered the best preventive measure.
- Bone mineral content declines during the post-reproductive period in both men and women, but the decrease is significantly greater in women.
- Estrogen promotes bone growth by stimulating osteoblast activity and inhibiting osteoclast activity. Thus, at menopause, the loss in bone mineral content that normally occurs between the ages of 25 and 50 begins to accelerate.
- Excess bone loss can result in osteoporosis and a significantly increased risk of bone fracture; 80% of all individuals with osteoporosis are women.
- Exercise and dietary calcium, and vitamin D can affect bone mineral content. Although increasing the level of physical activity and dietary calcium after menopause has proved effective in slowing bone mineral loss, their combined effect is modest and has only a minor impact on the development of osteoporosis
- The primary preventive measure for osteoporosis is to encourage women between the ages of 14 and 30 to increase their level of exercise and their intake of calcium to achieve the greatest possible peak bone mass.
本章结束