8.1 身体组成和能量代谢的变化
The shape and composition of the human body reflect, for the most part, the relationship among the amounts of its four primary constituents: water, 蛋白质, lipid, and bone. Although lifestyle and personal choices can have a major impact on body composition, the amounts of 蛋白质, lipid, and bone are also influenced by the physiological stage of life (the percentage of water in the body remains remarkably consistent throughout life).
From infancy through puberty, the body focuses on the growth and development of its internal organs, bones, and cells of the immune system, and the rate and amount of 蛋白质 deposition are higher during this period than at any other time in the life span. Prior to puberty, the shape and composition of the human body do not differ significantly between the sexes, but the onset of puberty initiates a greater focus on the growth of sex-linked characteristics. Muscle development in males outpaces that in females, while females generate greater fat deposition. Both sexes experience significant growth in bone mass, proportional to their final body height. The shape and composition of the human body during growth and development have a strong genetic component, but as the current epidemic of childhood obesity demonstrates, environmental influences are also important.
Once growth and development have ended—somewhere between 25 and 30 years of age—the size, shape, and weight of the human body reflect, for the most part, factors over which we have direct control. While the normal, active, and developmentally mature adult experiences a slight age-related decrease in the mass of muscle, internal organs, and bone, fat stores remain dynamic throughout life, increasing or decreasing depending on nutrition and exercise. Near the end of the life span, decreases in all components of the body accelerate.
In this section, we examine the normal age-related changes in the composition and size of the human body, along with the mechanisms that underlie these changes. We begin with a brief summary of how energy intake and expenditure affect the amount of fat we store. Then we look more closely at specific age-related alterations in body composition and weight.
8.1.1 Energy balance is the difference between intake and expenditure
Humans, like all organisms, need energy to drive the basic chemical reactions of life. Our energy comes from the food we eat in the form of fat and carbohydrate. (Humans do not, to any great degree, use 蛋白质 as an energy source, except during starvation.) The biochemical mechanisms by which fat and carbohydrate give rise to ATP, the cellular form of energy, were detailed in Chapter 4. Here we look at ways to evaluate whether the combination of food intake (energy intake) and physical activity (energy expenditure) leads to maintaining, losing, or gaining weight. We begin by calculating energy balance, using Equation 8.1
Energy balance = energy intake – energy expenditure
Our energy intake is easily determined by calculating the amount of energy in the fat, 蛋白质, and carbohydrate of the food we eat. This energy is measured in joules. A joule (J) is defined as the energy expended in applying a force of 1 newton through a distance of 1 meter. Because scientists are concerned with large amounts of energy, food energy is generally expressed in kilojoules (kJ): 1 kJ = 10 3 J. You might also see food energy expressed in kilocalories (kcal), an older convention that is still often used. A calorie is the amount of energy required to heat 1 gram of water 1°C (1 kcal = 10 3 cal). The conversion factors for kilojoules and kilocalories are 1 kJ = 0.239 kcal, and 1 kcal = 4.184 kJ. TABLE 8.1 shows the energy content of the four macronutrients in food types: fat, 蛋白质, carbohydrate, and alcohol. By summing the total amount of energy of the macronutrients in food we consume in a day, we can determine our energy intake for the day. Although 蛋白质 and alcohol are not generally used as starting substrates for producing ATP, they do have the potential to be converted to fat and carbohydrate and stored in the body's energy reserves, and thus they must be included in the calculation of energy balance.
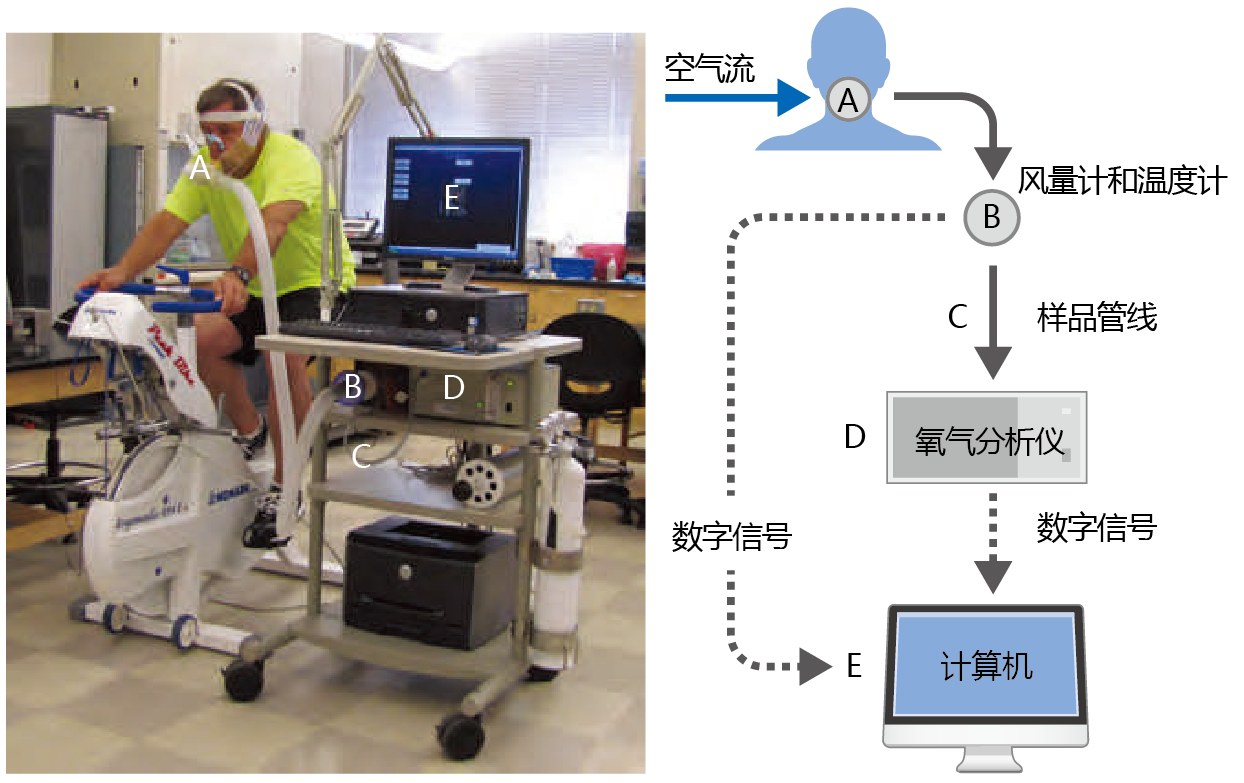
Determining energy expenditure is a bit more complicated and is normally accomplished through indirect calorimetry, a calculation of energy expenditure based on the measurement of respiratory gases (Figure 8.1). Total energy expenditure (TEE) includes three components: resting energy expenditure, physical activity, and diet-induced thermogenesis (Equation 8.2). TEE is also measured in kilo joules or kilocalories.
Total energy expenditure (TEE) = resting energy expenditure (REE)+
physical activity+ diet-induced thermogenesis (DIT) (8.2)
Figure 8.1 Indirect calorimetry. Oxygen consumption by the whole body can be determined through an analysis of respiratory gases. (A) The subject breathes through a one-way valve, which forces air to move in one direction (solid arrows). (B) The expired air travels through a hose to a device that measures its volume and temperature. (C) A sample of the expired air goes to the oxygen analyzer (D); the most common type of oxygen analyzer heats the air to a temperature that causes ionization of the oxygen molecules. (E) An ionized-oxygen detector inside the analyzer sends a digital signal (dotted lines) with information on the raw oxygen amount to a computer. The computer calculates the actual oxygen amount by adjusting the raw amount based on the temperature of the expired air. Subtracting the amount of expired oxygen from the amount of inspired oxygen gives the oxygen consumption. Multiplying the oxygen consumption (in liters) by 20.92 kJ gives a good estimate of energy expenditure. (Photo courtesy of Jennifer Ruhe.)
Resting energy expenditure (REE) is the amount of energy required to maintain the essential functions of life—heart rate, body temperature, brain function, and so on—and makes up 60–70% of TEE. Physical activity includes all movement of skeletal muscles, no matter how slight, and, on average, contributes about 20% to TEE in the adult human. However, the contribution of physical activity to TEE varies significantly among individuals. For example, a highly trained endurance athlete may expend as much 30% of his or her TEE on exercise, whereas a truly sedentary individual may expend only 5% of TEE on physical activity. Diet-induced thermogenesis (DIT) is the amount of energy required for digestion, absorption, and nutrient storage and accounts for the remaining 10–20% of TEE. The contribution of DIT to TEE does not vary much among individuals or with age, is difficult to measure, and is normally included as a constant in the TEE equation.
8.1.2 Accumulation of fat occurs throughout maturity
The typical mature human body contains almost 40 days‘ worth of energy in the form of fat, whereas we store only about 1 day‘s worth of energy in the form of glucose. Thus, when we measure the energy state of the mature human body—the energy balance—we are actually measuring the dynamics of fat storage. Positive energy balance—greater energy intake than expenditure—results in an increase in fat storage and in body weight. Negative energy balance—greater expenditure than energy intake—results in decreased fat storage and body weight. A person is said to be in energy balance when intake and expenditure are equal. In this case, body weight does not change.
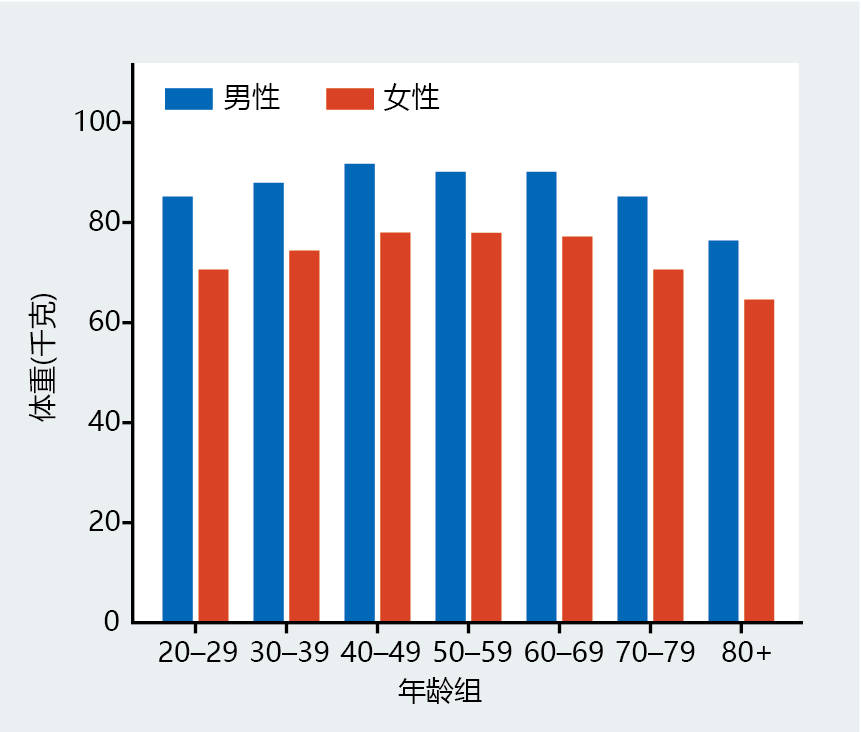
So, once we have attained full growth and development—that is, maturity—changes in our body weight reflect alterations in the amount of fat we store. Data collected from the ongoing National Health and Nutrition Examination Survey III (NHANES III) show that body weight increases, on average, by approximately 15% between the ages of 20 and 60–69 (Figure 8.2). The increase in weight occurs slowly, as small changes in energy balance over long periods have large effects on body weight. We can use a simple example to demonstrate the impact of small changes in energy balance sustained over long periods on the storage of fat. Consider a woman weighing 50 kg (about 100 pounds) with 10 kg of stored fat, equivalent to 389,000 kJ of energy (38.9 kJ/g × 10,000 g; see Table 8.1). This woman is currently in energy balance, with a daily food intake of 8370 kJ and a constant and stable REE and DIT of 5857 kJ and 837 kJ, respectively. Using Equation 8.2, we can calculate the amount of energy she uses per day in physical activity (Equation 8.3) .
Total energy expenditure (TEE) = 8370 kJ
Resting energy expenditure (REE) = 5857 kJ
Diet-induced thermogenesis (DIT) = 837 kJ
Thus,
Physical activity = TEE – REE – DIT= 8370 kJ – 5857 kJ – 837 kJ = 1676 kJ
| BOX 8.1 BODY MASS INDEX AND MORTALITY RISK |
|
The body mass index (BMI), the ratio between weight and height (Equation 8.4), can be another useful way to describe changes in fat content. Since genetics plays a large role in determining one‘s final stature, and height generally remains stable when growth and development are complete, BMI is a more sensitive and individualized measure of body fat than just weight alone. More importantly, BMI has been shown to be highly correlated with mortality due to health problems associated with being underweight, overweight, or obese (Figure 8.4). BMI = weight (kg) / height 2 (m 2) The calculation of BMI dates back to the early 1800s, when a Belgian social scientist, Adolphe Quetelet (1796–1874), found that body weight during growth varied as a function of height squared. The index, then called the Quetelet index, had limited use as a measurement relating obesity to health, primarily because obesity was virtually unknown in the general population at that time. It was not until the end of World War II that statisticians working for life insurance companies noted a slight increase in mortality rates among individuals weighing more than the average body weight for the population. This led to the development of the weight-to-height tables and the concept of an ideal body weight for a specific height. It was soon found that the large variation among individuals in what constituted an ideal body weight rendered the weightto-height tables too inaccurate for use by physicians as a measure of health.
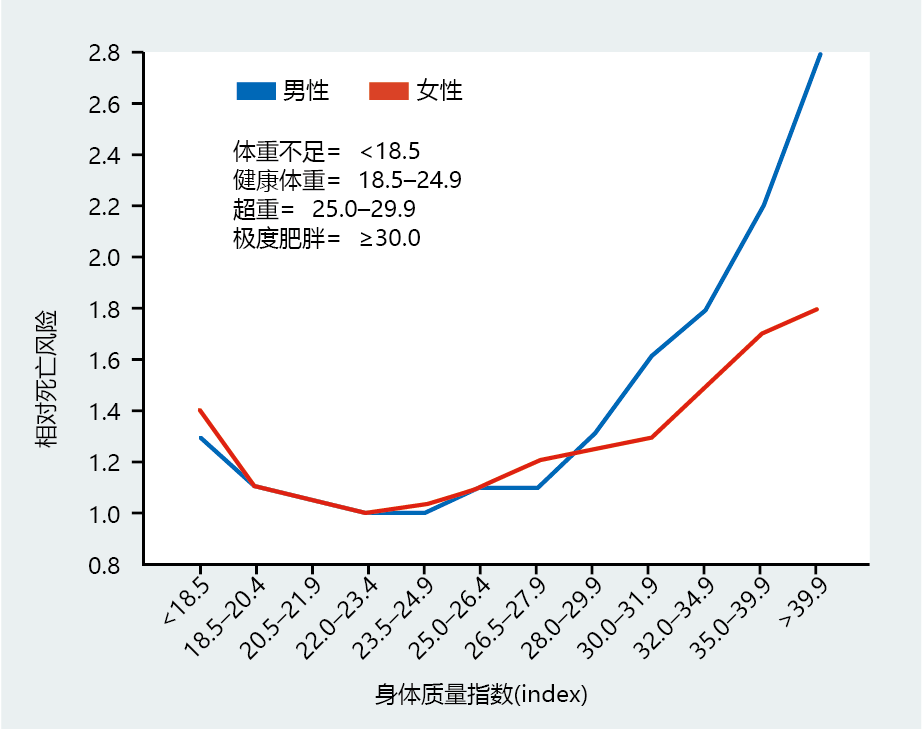
In 1972, Ancel Keys (1904–2004) was the first to note that the Quetelet index was the best proxy for body fat and suggested its use as an easy method for physicians to discuss possible health problems associated with obesity. Keys popularized the name “body mass index.” The results of several investigations conducted during the last two decades of the twentieth century showed a close relationship between BMI and the risk for health problems. These findings led the National Institutes of Heath (NIH) to establish specific BMI values as guidelines for healthy weight (shown in Figure 8.4). Figure 8.4 Relationship between body mass index (BMI) and relative risk of death. These graphs, based on data from 457,758 men and 588,369 women, collected between 1984 and 1996, clearly show that the risk of death is greater for those who are underweight or overweight. The BMI categories (listed above the curves) are commonly used as age-independent markers for possible health problems associated with fat content in otherwise healthy adults over the age of 20. (Adapted from E.E. Calle et al., N. Engl. J. Med. 341:1097–1105, 1999. With permission from New England Journal of Medicine.)
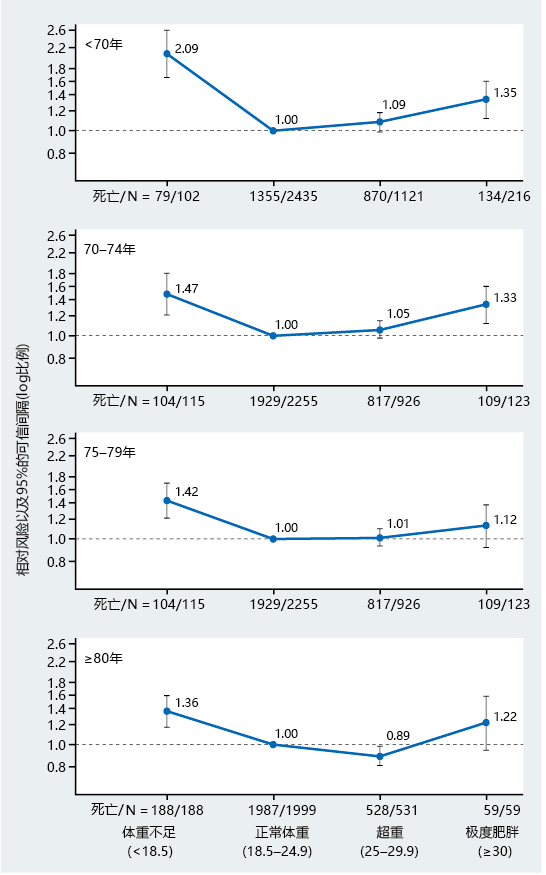
It has become clear that the NIH's BMI values need to be adjusted for the older population. Several longitudinal studies have found that BMIs in the range of 25–28 (a range considered overweight and with higher risk for health problems, according to NIH guidelines) do not increase health risk for those over the age of 75 (Figure 8.5). However, BMIs of less than 18.9 (considered underweight) remain a risk factor for health problems in the elderly. Most clinical experts agree that in the older population, being under-weight poses a greater risk for health problems than being obese. Many clinicians have stated that individuals older than 75 who are within the 25–30 BMI range should not consider a weight-reduction plan, except for vanity reasons, and should never drop below a BMI of 22. Figure 8.5 Relationship between BMI and relative risk of death in age groups between 45 and 101. Note the progressive decline in relative risk in the overweight category from ages <70 years to ≥80 years. Many experts believe that the older population should have a different set of BMI values from those used for the general population, to reflect these findings and to help prevent underweight. This and many other investigations find that underweight (BMI <18.9) and obesity (BMI ≥30) remain risk factors for early mortality in the older population. Deaths/N, on the horizontal axes, indicates number of deaths in the sample size N for each BMI category. (From M.M. Corrada et al., Am. J. Epidemiol. 163:938–949, 2006. With permission from Oxford University Press.)
|
Figure 8.2 Average weights of men and women in the United States in 2004. These data are from the most recent year of a large-scale (19,000 participants) study that includes individuals over the age of 70. Cross-sectional studies completed since 2004 have supported these data. (Data from M.A. McDowell et al., Natl Health Stat. Rep. 10:1– 48, 2008.)
If the woman begins to eat a little more each day, say just 418 kJ (equal to about ¼ cup or 3 tablespoons of vanilla ice cream) while keeping her physical activity the same, her energy balance becomes positive and she begins to store fat. Thus, in approximately 100 days she will gain about1 kg of body weight, and in 1 year she will gain almost 4 kg (1 kg of body fat is equivalent to about 38,900 kJ). Thus, even small changes in energy intake can have a significant impact on body weight over the long haul. Similarly, slight changes in energy expenditure would have the opposite effect. An increase in physical activity of 418 kJ daily, such as jogging at a moderate pace for 1 mile (or walking 1.5 miles), would bring the woman back into energy balance and prevent fat accumulation.
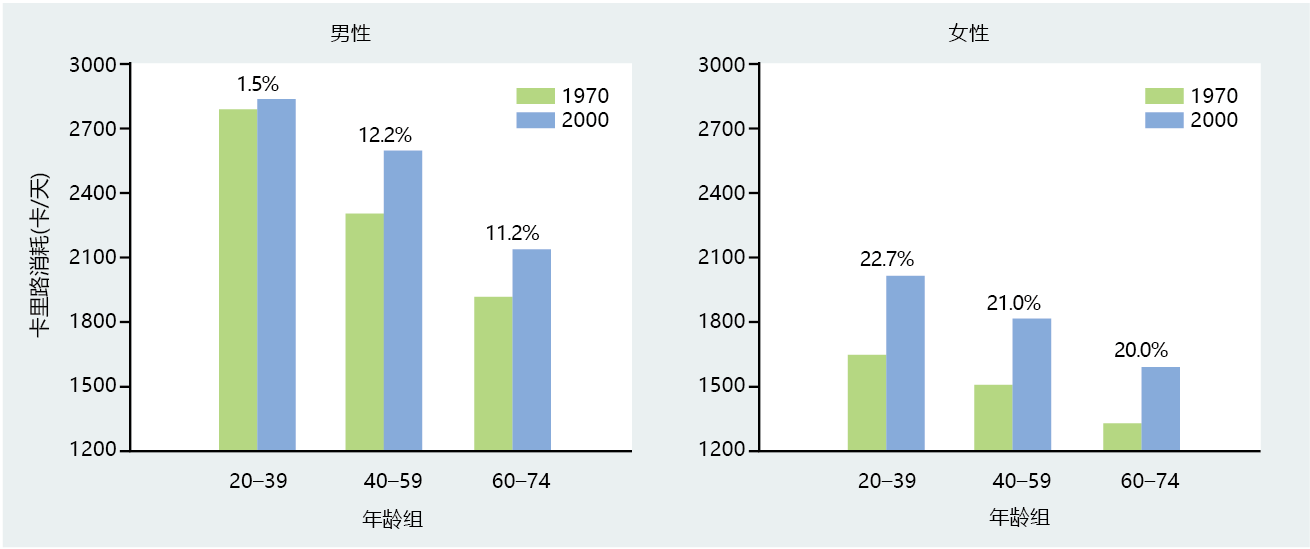
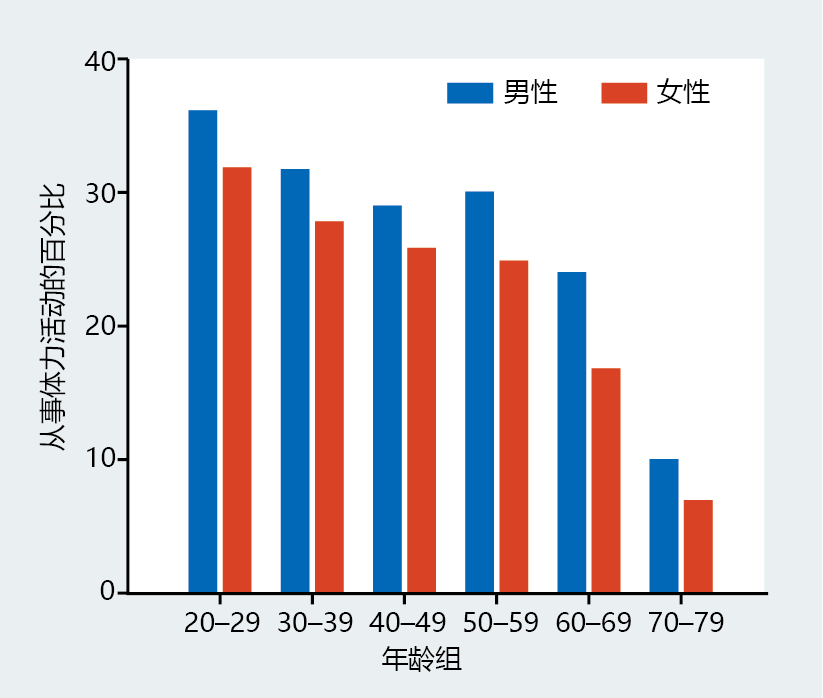
As indicated by this example, fat accumulation can result from excessive calorie intake, decreased physical activity, or a combination of the two. Aging affects both of these. (BOX 8.1 describes a useful way of considering changes in body fat with age.) Calorie consumption tends to decrease with age (Figure 8.3) —although, as Figure 8.3 shows, it increased, overall, by an average of 11% in men and 22% in women between 1970 and 2000, and data from recent cross-sectional investigations suggest that calorie consumption continues to increase. Despite this increase in calorie consumption in recent years, the agerelated decrease remains. In addition, older individuals are less likely than younger people to engage in voluntary physical activity (Figure 8.6). Since energy intake seems to decrease with age, the only logical explanation for the age-related increase in body weight is that the decrease in energy expenditure over time must be greater than the decrease in energy intake, a conclusion supported by the data in Figure 8.6. The lack of physical activity can also lead to a loss of muscle tissue exceeding that expected for normal age-related skeletal muscle loss (a condition known as sarcopenia, discussed later in the chapter). The loss of muscle mass due to physical inactivity leads to a decrease in REE, exacerbating the age-related decrease in energy expenditure. After age 70, the body weight loss most likely reflects an association with decreased calorie intake near the end of life, as discussed later.
Figure 8.3 Average calorie consumption by men and women in various age groups in 1970 and 2000. Numbers above the bars are the percentage increase between 1970 and 2000. (Data from J.D. Wright et al., Mortal. Morbid. Wkly Rep. 53:80–82, 2004.)
Figure 8.6 Percentage of individuals engaging in regular leisure-time physical activity sufficiently vigorous to affect the mass of body fat. Regular leisure-time physical activity is defined as engaging in vigorous physical activity for 30 minutes or more five or more times per week or engaging in light to moderate physical activity for 20 minutes or more three or more times per week. (Data from J.R. Pleis, B.W. Ward, and J.W. Lucas, Vital Health Stat. 10:217, 2010; C.A. Schoenborn, J.L. Vickerie, and E. Powell-Griner, Health Characteristics of Adults 55 years and Over: United States, 2000–2003, Hyattsville, MD: National Center for Health Statistics, 2006.)
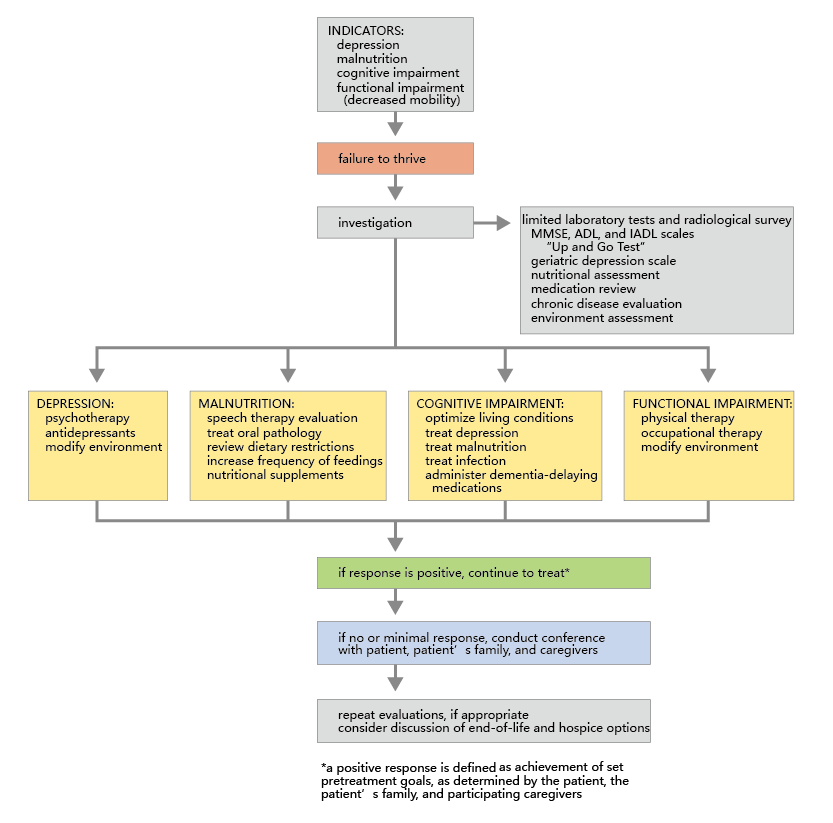
Figure 8.7 An algorithm used by physicians to diagnose and treat patients with geriatric failure to thrive. MMSE = mini mental state examination; ADL = activities of daily living; IADL = instrumental activities of daily living. (From R.G. Robertson and M. Montagnini, Am. Fam. Physician 70:343–350, 2004. With permission from American Academy of Family Physicians.)
8.1.3 Excessive loss of body weight near the end of the life span increases mortality rate
Although body weight increases throughout much of the human life span, there comes a time when weight begins to decline. This can be seen in Figure 8.3, where the body weight of those 70 and older is less than that in the younger age groups. The decreased body weight in this age group reflects the inclusion in the data of individuals near the end of their life span. End-of-life weight loss has only recently been accepted as an age-related phenomenon, and the underlying mechanism has not yet been identified. We do know, however, that both fat and muscle mass seem to decline during this period.
Recent data suggest that a decrease in food intake parallels the end of-life decline in body weight and can lead to a clinical condition known as the anorexia of aging. The four hallmarks of the anorexia of aging—excessive weight loss, decreased appetite, poor nutrition, and inactivity—are the primary predictive symptoms of a larger and more general syndrome known as geriatric failure to thrive. This multi-factorial syndrome, often indicating the end of life, includes impaired physical function, malnutrition, depression, and cognitive impairment. An algorithm for diagnosing geriatric failure to thrive has been established and suggests when physicians might begin discussing end-of-life options with patients and families, to prevent needless interventions that may only prolong suffering (Figure 8.7).
8.1.4 Sarcopenia is the age-related decline in skeletal muscle mass
An age-related decrease in muscle mass, known as sarcopenia, occurs during the maturity phase of the human life span. The decrease happens regardless of factors known to increase muscle mass, such as increased physical activity. The loss in muscle tissue with age reflects a decrease in both muscle cell number and cell size, and it seems to be greater in men than in women. The loss in both cell number and size differentiates sarcopenia from loss of muscle mass due to disuse, in which only cell size decreases. A series of cross-sectional and longitudinal studies have shown that after the age of 40, muscle mass declines at a rate of about 2–3% per decade in men and 1–2% per decade in women.
The mechanism underlying sarcopenia is mostly unknown, although some changes are consistently observed in studies investigating the causes of sarcopenia. Fat deposits and connective tissue seem to replace the contractile components of muscle. Since only myocytes (muscle cells), or muscle fibers, can generate force, increased fat and connective tissue in the muscle will decrease strength.
The type of muscle fiber affected by sarcopenia appears to be selective. Muscle cells are classified based on their content of isoforms of the contractile 蛋白质 myosin. Cells with high concentrations of the myosin isoform that results in slow contraction are known as type I fibers (sometimes called slow-twitch fibers). Muscle fibers with high concentrations of the myosin isoform that results in fast contractions are known as type II fibers (fast-twitch fibers). The sarcopenia-related muscle fiber loss seems to have a greater effect on type II fibers than type I. Thus, muscles that require a high speed of contraction, such as those in the hands and other areas of fine motor control, tend to be more affected by sarcopenia than the large muscle groups. Interestingly, recent investigations have discovered a third type of muscle fiber, type IIX, that appears only during aging. It has characteristics of both type I and type II fibers. The role of type IIX fibers in sarcopenia has yet to be investigated.
A recent observation made in rodents, as models for human aging, is that the number and function of neuromuscular junctions, or motor end plates, decline with age. The motor end plates regulate how many muscle fibers are used during a contraction: the greater the number of motor end plates recruited by the nerve innervating the muscle, the greater the strength of the contraction. Thus, the age-related decline in motor end plates may lead to fiber disuse and signal the start of apoptosis. Direct evidence for disuse and apoptosis in sarcopenia in humans has yet to be published, but several investigations on completely sedentary young adults (experimentally induced bed rest) and individuals returning from extended stays in space (zero gravity) show apoptotic events related to a decline in motor end plate activity.
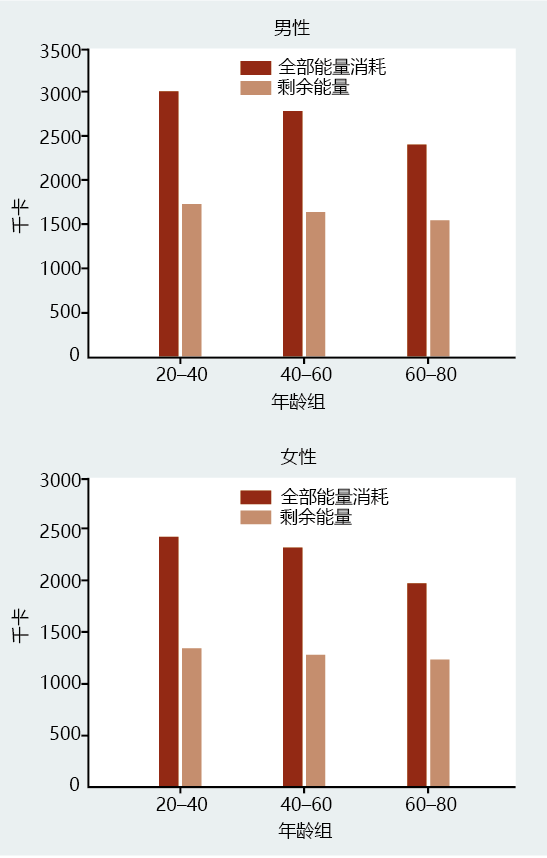
The loss of muscle tissue can have significant health consequences. Muscles use considerable amounts of energy at rest to maintain their form and to stay prepared for contraction. The muscles use more than half of REE. Thus, a decrease in muscle mass reduces resting metabolic rate, and without an equivalent reduction in energy intake, this leads to fat accumulation. Men experience an approximately 2.5% decrease in resting metabolic rate per decade, whereas women seem to have a slower rate of decline, at 1.5% per decade (Figure 8.8). These values are remarkably close to the age-related loss in muscle mass. Lack of physical activity will lead to a greater loss in muscle tissue and accelerate the age-related drop in REE.
Figure 8.8 Total and resting energy expenditure at various ages in men and women. (Data from S.B. Roberts and G.E. Dallal, Public Health Nutr. 8:1028–1036, 2005.)
The primary job of human skeletal muscles is to provide strength and stability to the body. If muscle mass declines, one‘s ability to react to situations requiring a certain level of strength and stability will also decline. Consider the simple act of walking. We don‘t really think much about it until we take a misstep off a curb or step onto an uneven surface. During young adulthood, an injury from this misstep is unlikely, because we have enough muscle mass to react accordingly and maintain balance. With the age-related decline in muscle mass, an individual may have insufficient strength to keep upright when the misstep occurs. Indeed, falls resulting from the age-related decline in muscle mass are a major risk factor for morbidity and mortality.