9.9 未来之路和基本概念
The medical and research community has focused, in large part, on two mechanisms to combat chronic disease: reducing risk and delivering better treatment after diagnosis. This approach was highly successful during the latter half of the twentieth century in reducing the incidence of the top 10 causes of death and preventing the disability that often accompanies chronic disease. In recent years, this approach has begun to lose its effectiveness, as the incidence of many diseases, including heart disease and cancer, has been showing very small changes over time. Many believe that a fundamental shift in the research focus on chronic disease is warranted. To this end, the biogerontological community has long been calling for a new approach, from one with the exclusive focus on curing disease to one that also includes a focus on the mechanism(s) underlying aging. Such an approach reflects one simple and indisputable fact: aging is the number 1 risk factor for most chronic diseases. A discussion in Chapter 11 expands on this topic. Slowing down aging will delay or prevent many chronic diseases and extend the healthy life span (Figure 9.43).
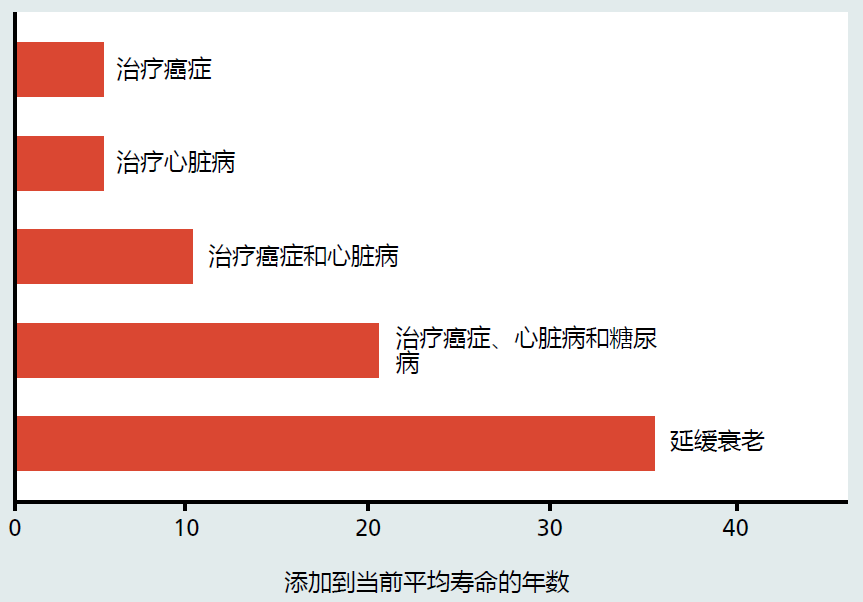
Figure 9.43 Benefits to average life span by focusing research on slowing the rate of aging as opposed to curing the leading causes of death. Data represent an aggregate of estimates published in various sources. (Adapted from original design by Miller RA. 2002. Milbank Q 80:155–174.)
The first step in reducing the burden of disease through slowing the rate of aging will be to gain a deep understanding of the multiple mechanisms of aging and how they interact. Due to the random nature of aging, we can expect that every individual will have a different path to aging, that is, different mechanisms, and that path may lead to a variety of diseases. Using a reductionist or disease-centered approach to evaluate mechanisms underlying a process as complex as aging will be an inefficient use of resources and research time. Rather, complex biological problems call for new and innovative research methods. Gaining a deeper understanding of how slowing the rate of aging will lessen the impact of chronic disease will come through a greater use of the new techniques associated with personalized medicine (Chapter 1) and systems biology (Chapter 2).
ESSENTIAL CONCEPTS
• The human nervous system is composed of the CNS, consisting of the brain and spinal cord, and the PNS, consisting of all other nerves outside the CNS.
• Neural cells (neurons) are made up of three basic components: dendrites, cell body, and axon.
• Neurotransmission is propagated by establishment of an action potential, a brief depolarization of a small section of the nerve cell membrane.
• Neurotransmitters relay electrical signals from one neuron to another across synapses. A synapse is made up of the axon terminal of the presynaptic neuron, dendrite of the postsynaptic neuron, and synaptic cleft.
• Time-dependent changes in the human brain are minor and do not seem to significantly affect brain function.
• Accumulation of two protein aggregates, amyloid plaques and neurofibrillary tangles, in the human brain appears to be a normal time-dependent phenomenon.
• The cause of Alzheimer's disease is unknown, but individuals with Alzheimer's are found to have high concentrations of amyloid plaques and neurofibrillary tangles.
• There are three general forms of Alzheimer's disease: early onset, late onset, and familial. Early onset and familial Alzheimer's are genetic in origin, whereas the late-onset form does not seem to be inherited.
• Cerebral spinal fluid levels of Aβ 42 , total tau, and hyperphosphorated tau may be early biomarkers for Alzheimer's disease. MRI and PET provide visualization of possible biomarkers and help to confirm a diagnosis of Alzheimer's disease.
• Parkinson's disease results from the loss of dopamine-producing neurons in the substantia nigra region of the basal ganglia.
• The heart consists of two separate pumps: the right side delivers oxygen-poor blood to the pulmonary system (lungs); the left side supplies oxygen-rich blood to the body.
• The muscle of the heart and arteries is excitable tissue. That is, the muscle generates action potentials in response to neural and hormonal stimulation.
• Cardiac output is determined by the amount of blood returned to the heart. Stretching of the heart muscle in response to venous return determines the force necessary to eject blood from the ventricles.
• Arterial plaques, accumulations of cholesterol-filled fatty deposits in the arteries, are present in 100% of the aged population. Excess accumulation of arterial plaques results in the disease atherosclerosis.
• Age, smoking, hypertension, and hyperlipidemia are the major risk factors for coronary artery disease.
• More than 50% of individuals 65 years and older have hypertension (high blood pressure), defined as a consistent systolic blood pressure of ≥130 mm Hg or diastolic pressure of ≥90 mm Hg.
• Heart failure can be defined as the inability of the myocardium to generate the contractile force needed to eject the blood volume required for the oxygen demands of the body—that is, an abnormal decrease in cardiac output.
• Blood glucose is maintained within a narrow range of 90–120 mg/dL by the competitive action of two hormones produced by the endocrine cells of the pancreas: insulin and glucagon. This level of blood glucose must be maintained because the brain uses only blood glucose for its energy needs.
• Insulin facilitates the uptake of glucose into cells by initiating an intracellular signaling cascade. Insulin can also regulate the metabolism of fats and proteins.
• Insulin resistance is the inability of insulin to effectively stimulate glucose uptake into cells. It is a major risk factor for type 2 diabetes.
• One result of type 2 diabetes is damage to microvascular blood flow. Without proper blood flow, tissue can be damaged, leading to tissue injury or tissue death.
• Estimates indicate that more than 80% of new cases of type 2 diabetes are related to obesity. Maintaining a healthy weight is considered the best preventive measure.
• Bone mineral content declines during the postreproductive period in both men and women, but the decrease is significantly greater in women.
• Estrogen promotes bone growth by stimulating osteoblast activity and inhibiting osteoclast activity. Thus, at menopause, the loss in bone mineral content that normally occurs between the ages of 25 and 50 begins to accelerate.
• Excess bone loss can result in osteoporosis and a significantly increased risk of bone fracture; 80% of all individuals with osteoporosis are women.
• Weight-bearing exercise, dietary calcium, and vitamin D can affect bone mineral content. Although increasing the level of physical activity and dietary calcium after menopause has been shown to be effective in slowing bone mineral loss, their combined effect is modest and has only a minor impact on the development of osteoporosis.
• The primary preventive measure for osteoporosis is to encourage women between the ages of 14 and 30 to increase their level of exercise and their intake of calcium to achieve the greatest possible peak bone mass.
本章结束


