第10讲 Immunological Memory
HEADS UP!
The innate immune system has a "hard-wired" memory which allows it to remember encounters with invaders from the ancient past. The adaptive immune system has an "updatable" memory which remembers the specific invaders we have encountered during our lifetime. Memory B and T cells have received "upgrades," and are better able to deal with a second attack than are the B and T cells which responded to the initial invasion. Some innate system cells can be "trained" to respond more strongly to a subsequent threat.
INTRODUCTION
One of the most important attributes of the immune system is that it remembers past encounters with attackers.
These memories help protect against future challenges.
Both the innate and the adaptive systems have memories, but what these two systems remember is quite different.
INNATE MEMORY
The innate immune system has a "hard-wired" memory which is extremely important in defending us against everyday invaders. This memory is the result of millions of years of experience, during which the innate system slowly evolved genes for receptors that can detect the signatures of common invaders. These receptors (e.g., Toll-like receptors) usually detect molecular structures which are essential for an invader's lifestyle, and which are characteristic of broad classes of microbial pathogens (e.g., all bacteria that have LPS as a cell membrane component). Moreover, these receptor genes are passed down from generation to generation, and do not change during the lifetime of a human. This ancient memory allows an immediate and robust response to invaders that have been attacking humans for a very long time. Importantly, although the innate immune memory is "tuned" to past invaders, the innate immune system also can protect us against new invaders (for example, viruses that enter the human population from wild animals) if these novel pathogens have structural features in common with ancient invaders.
Some cells of the innate system (e.g., macrophages and NK cells) can be "trained" by a first exposure to a pathogen to respond more quickly and powerfully to a subsequent invasion. The hyperactivation of a macrophage is an example of such training. Although the rules that govern this " trained immunity " are still being worked out, in humans this type of memory usually seems to be non-specific. That is, the initial defense against one pathogen can train innate system warriors to respond more vigorously against a subsequent attack by the same or a different pathogen. In this way, trained immunity can help provide broad, non-specific protection against future microbial attacks. Trained immunity is usually shortlived, lasting only for weeks or months. And it is local.
Only the innate cells in the area of the original infection can be trained.
There is also some experimental evidence that natural killer cells which respond to an infection by the human cytomegalovirus can be trained to respond specifically to a subsequent attack by this virus. Of course, the human cytomegalovirus is older than dirt. It has been infecting humans for a very long time. Consequently, we shouldn't be surprised if this virus appears in the NK cell's "list" of ancient invaders. Nevertheless, questions still remain about the specificity of this training, because the cytomegaloviral antigen that human NK cells might be recognizing has not been identified.
ADAPTIVE MEMORY
The innate immune system uses hard-wired receptors to "remember" broad classes of pathogens which also plagued our ancestors. In contrast, the adaptive immune system is set up to remember the specific attackers we encounter during our lifetime. Although B and T cells have a diverse collection of receptors that can recognize essentially any invader, there are relatively few naive B or T cells with receptors that can recognize any particular attacker – not enough to mount an immediate defense.
So in practical terms, B and T cells really begin life with a blank memory. During an initial attack, pathogen-specific B or T cells proliferate to build up their numbers.
Then, when the invader has been subdued, most of these cells die off, but some (typically a few percent) remain as memory B or T cells to defend against a subsequent attack by the same invader.
B cell memory
It is clear that B cells and the antibodies they produce can confer life-long immunity to infection. For example, in 1781, Swedish traders brought the measles virus to the isolated Faroe Islands. In 1846, when another ship carrying sailors infected with measles visited the islands, most people who were older than 64 years did not contract the disease – because they still had antibodies against the measles virus. Even the longest lived antibodies (IgG) have a half-life of less than a month, so antibodies would have to be made continuously over a period of many years to provide this long-lasting protection.
When B cells are activated during the initial response to an invader, three kinds of B cells are generated. First, short-lived plasma B cells are produced in the lymphoid follicles of secondary lymphoid organs.
These cells travel to the bone marrow or spleen and produce huge quantities of antibodies that are specific for the attacker. Although they only live for a few days, short-lived plasma B cells produce antibodies which are extremely important in protecting us against an enemy that the adaptive immune system has never encountered before.
In addition to short-lived plasma B cells, two types of memory B cells are produced in germinal centers during an invasion. Importantly, the generation of both types of memory cells requires T cell help. The first kind of memory B cell is the long-lived plasma cell. In contrast to short-lived plasma cells, which are generated rapidly after infection and which die after a few heroic days, long-lived plasma cells take up residence in the bone marrow, which provides a supportive environment that allows these plasma cells to survive for a long time.
Importantly, long-lived plasma cells continually produce modest amounts of antibodies – antibodies that can provide life-long immunity to subsequent infections. So together, short-lived and long-lived plasma B cells provide both immediate and long-term antibody protection against attacks.
The second type of memory B cell is the central memory B cell. These cells reside mainly in the secondary lymphoid organs, and their job is not to produce antibodies.
Central memory B cells function as memory "stem cells" which slowly proliferate to maintain a pool of central memory B cells, and to replace long-lived plasma cells that have died of old age. In addition, if another attack occurs, central memory cells can quickly produce more short-lived plasma B cells.
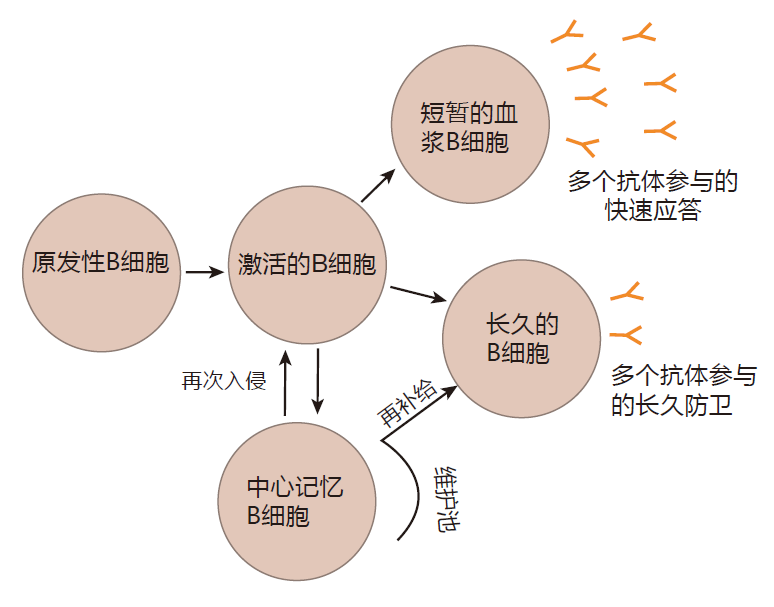
This strategy, which involves three types of B cells, makes good sense. When an invader first attacks, antibodies need to be made quickly to tag invaders for destruction. That's what short-lived plasma B cells do.
If, at a later time, the pathogen attacks again, it is important to already have invader-specific antibodies on hand that can provide an immediate defense. That's the job of long-lived plasma B cells. And between attacks, readiness is maintained by central memory B cells. These cells replenish supplies of long-lived plasma cells, and also stand ready to produce a burst of short-lived plasma B cells – cells that can rapidly manufacture large quantities of invader-specific antibodies. How a baby B cell "decides" what to be when it "grows up" – a short-lived plasma B cell, a long-lived plasma cell, or a central memory B cell is unknown.
T cell memory
T cells also are able to remember a previous encounter with an invader. Although T cells can be activated either with or without assistance from helper T cells, only Th-dependent activation of T cells generates memory T cells.
T cell memory is similar, but not identical, to B cell memory. After naive T cells have been activated in response to an initial attack, and have proliferated to build up their numbers as much as 10,000-fold, many of them are given passports to travel out to the tissues to do battle with the enemy. These are the effector T cells. After the attack has been repulsed, about 90% of the effector T cells die by apoptosis, but some of them, the tissue- resident memory T cells, remain in the tissues near the site of the original encounter with the pathogen. There they wait for a subsequent infection in which the same pathogen breaches the barrier defenses and enters the tissues. If that attack occurs, they rapidly reactivate, proliferate a bit, and begin to destroy the invaders they remember. Other T cells which responded to the initial infection become effector memory T cells.
These cells circulate through the blood and lymph and are "on guard" in case there is a subsequent attack anywhere in the body. Finally, some memory T cells remain in the secondary lymphoid organs. These are the central memory T cells. During a subsequent attack, central memory T cells can activate quickly. After a brief period of proliferation, most mature into effector cells, which join effector T cells at the battle scene. The rest of the central memory T cells remain in the secondary lymphoid organs and wait for another attack by the same invader.
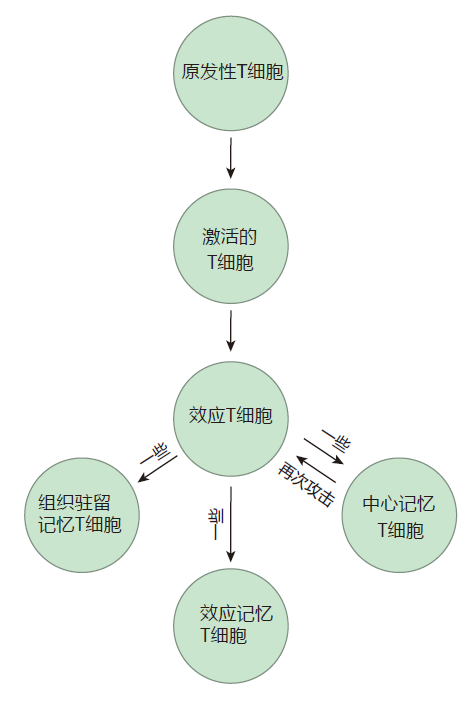
This three-pronged strategy works well. If invaders return to infect the same area of the body, the tissueresident memory T cells are there to greet them. On the other hand, if the invaders attack a different part of the body, the effector memory T cells are patrolling those areas to provide protection. And the central memory T cells are standing by in the secondary lymphoid organs to provide backup. It is not known how long each type of memory T cell persists after an attack, but altogether, T cell memory usually lasts about a decade.
Th1, Th2, and Th17 cells, which function to turn on the immune system, have long memories. In contrast, iTreg cells, which turn the immune system off once the battle has been won, have very short memories. This is a good thing. Long-lived memory iTregs could keep the immune
system "turned off," preventing it from springing into action during a subsequent infection.
PROPERTIES OF ADAPTIVE MEMORY CELLS
The adaptive immune system remembers specific invaders so well and reacts so powerfully during a subsequent infection that we usually don't even know we have been reinfected. There are a number of reasons why memory cells are better able to deal with a second attack than were the inexperienced B and T cells which responded to the original invasion. First, there are many more of them. Indeed, when we are attacked for the first time, there usually is only about one B or T cell in a million which can recognize that invader. In contrast, by the time the battle is over, the memory pool of pathogen-specific cells will have expanded so that usually about one in a thousand of all the B or T cells will recognize the attacker. Consequently, the adaptive immune system's response to a subsequent attack is much more robust than the initial response – in part because there are so many more invader-specific cells "on duty."
In addition to being more numerous than their inexperienced predecessors, memory B and T cells are easier to activate. For example, memory T cells can be activated by MHC–peptide concentrations that are as much as 50-fold lower than those required to activate virgin T cells. Also, during the reactivation of memory cells, recognition of cognate antigen still is required, but at least in some cases, co-stimulation is not essential.
Now why would it be advantageous to have a system in which it is difficult to activate B and T cells the first time, but relatively easy to reactivate them? Clearly, we want activation of virgin cells to be tightly controlled – because we only want to engage the adaptive immune system when there is a real threat. Consequently, a fail-safe activation requirement for virgin B and T cells is important.
On the other hand, once these cells have been through the stringent two-key selection for primary activation, we want them to respond quickly to a subsequent attack by the same invader. So making it easier for them to be reactivated is a great idea.
There is a third reason why memory B cells are better defenders than naive B cells: Most memory B cells are "upgraded" versions of the original, virgin B cells. These upgrades are of two types. First, during the course of an attack, B cells can switch the class of antibody they make from the "compromise" antibody class, IgM, to one of the other classes (IgG, IgA, or IgE) which specializes in dealing with that particular kind of invader. This class switch is imprinted on the memory of the B cells that remain after an attack. As a result, memory B cells are able to produce the antibody class which is just right to protect against the invader they remember.
Also, during an attack, B cells use somatic hypermutation to fine-tune both their receptors and the antibodies they manufacture. Somatic hypermutation results in upgraded B cell receptors that can detect small amounts of foreign antigen early in an attack. This allows central memory B cells to be activated quickly during a subsequent infection. Somatic hypermutation also results in long-lived plasma cells which make upgraded antibodies that can bind more tightly to the invader.
COMPARING B AND T CELL MEMORIES
B and T cell memories are similar in that both systems center around stem-cell-like central memory cells. These central memory cells reside in the secondary lymphoid organs, where they are strategically located to intercept invaders as they enter the body. Memory B and T cells are more potent weapons than naive cells because a larger fraction of them are specific for the invader they remember, and because they are easier to activate than virgin B and T cells.
Other aspects of B cell and T cell memory, however, are different. In response to an invasion, B cells can fine-tune their receptors through somatic hypermutation. T cells cannot. Moreover, there is no T cell equivalent of the long-lived plasma B cell. Once we have been exposed to a pathogen, long-lived plasma B cells continue to produce protective antibodies, frequently for a lifetime. Consequently, the weapons made by B cells (the antibody molecules) continue to be deployed even after an invasion has been repulsed. This works well because antibodies are very specific and rather benign. Only when they tag an invader is the rest of the immune system alerted to take action. So if the invader they recognize doesn't attack again, the antibodies produced by long-lived plasma B cells do nothing and cause no trouble.
In contrast, activated T cells produce cytokines and other chemicals that are non-specific, and which can cause severe damage to normal tissues. Consequently, it would be very dangerous to have T cells remain in action once an invasion has been repulsed. So instead of continuing to function after the enemy has been defeated, as long-lived plasma cells do, tissue-resident memory T cells and effector memory T cells go "dormant." If the attacker does not return, they cause no trouble. But if the enemy attacks again, these cells quickly reactivate and spring into action.
INNATE VERSUS ADAPTIVE MEMORY
Although both innate and adaptive immune systems remember, it is important to understand how these memories differ. The innate system remembers invaders that its hard-wired receptors recognize. Consequently, the innate memory is a static memory: It is not updatable – at least not on the time scale of a human lifetime. Although there will be slight genetic differences from person to person, all humans have essentially the same innate memory, which reflects the experience of the human race with common invaders that have been plaguing us for millions of years.
In contrast, the adaptive immune system has an expandable memory that can remember any specific invader to which we have been exposed, be it common or rare. Moreover, the adaptive immune system's memory is personal: Each of us has a different adaptive memory, depending on the particular invaders we have encountered during our lifetime.
Not only do we have different "lists" of invaders we have encountered, but even when two people have been attacked by the same microbe, their adaptive memories of that attack will be different – because the receptors on the collection of invader-specific B and T cells will differ from person to person. Indeed, because B and T cell receptors are made by a mix-and-match mechanism, no two humans will have the same adaptive memory.
REVIEW
Both the innate system and the adaptive system are able to remember past invaders. The innate immune system's memory is hard-wired, and depends on pattern-recognition receptors that have evolved over millions of years to identify common invaders. These receptors recognize signatures which are shared by classes of invaders, and focus on molecular structures that are not easily mutated.
In contrast, B and T cells of the adaptive immune system have updatable memories which can remember the individual invaders we have encountered during our lifetimes, both common and rare. Consequently, adaptive memory is personal in the sense that every person has a different adaptive memory.
Memory B and T cells are better able to deal with a second attack because they are much more numerous than before the first invasion, and because they are more easily activated than are virgin B and T cells. Moreover, memory B cells have receptors that have been fi ne-tuned by somatic hypermutation, and memory B cells usually have class switched to produce the type of antibody molecule which is most appropriate for the invader they remember.
As a result of these upgrades, memory B cells are more efficient at dealing with repeat offenders than were their virgin predecessors.
After a first attack, long-lived plasma B cells, which reside in the bone marrow, continuously produce moderate amounts of pathogen-specific antibodies.
These antibodies provide immediate protection if we are attacked again. The pool of long-lived plasma cells is continually replenished by central memory B cells, which proliferate slowly in the secondary lymphoid organs between invasions. If we are invaded again by the same pathogen, these central memory B cells quickly activate, proliferate, and most of them mature into plasma B cells – cells which can produce large quantities of pathogen-specific antibodies.
Tissue-resident memory T cells remain at the scene of the original battle and wait to "pounce" if we are attacked again in the same area of the body. Meanwhile, effector memory T cells circulate through the blood and lymphatic systems, patrolling for invaders which might pay a return visit at a different site. And central memory T cells persist in the secondary lymphoid organs following an attack. These cells proliferate slowly to maintain a pool of invader-specific T cells. Central memory T cells can react quickly to a second attack by proliferating and maturing into effector T cells, which can travel to the site of the invasion and destroy the enemy.
Some innate immune cells can be trained to respond more vigorously to a subsequent attack. In humans, this trained memory usually is non-specific, local, and not very long-lasting.


