8.6 CHANGES IN URINARY SYSTEM
The urinary system consists of two kidneys, two ureters, the bladder, and the urethra (Figure 8.40). With the exception of the kidneys, there are no significant time-dependent alterations in the system that impede the elimination of urine. Time-dependent urinary incontinence, the inability to control urination, is the result of abnormal muscle weakness, disease processes that affect the nerves controlling bladder function, or excessive urine production by the kidneys. Therefore, the focus here is on time-dependent changes in the kidney. We begin by examining normal renal function.
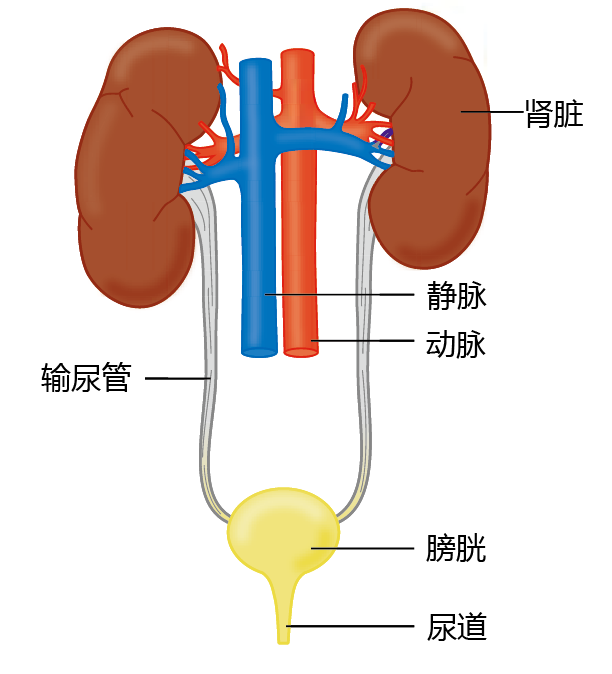
Figure 8.40 Anatomy of the human urinary system.
Kidneys remove metabolic waste products from blood
All human cells excrete metabolic waste product into the blood. The removal of either acetic or alkaline cellular waste is essential to maintaining the delicate balance of the blood pH, 7.2–7.4. Otherwise, the ability of the cell to carry out normal metabolic function would be affected. Maintenance of normal cell function also requires a stable blood concentration of certain minerals, collectively known as electrolytes, such as sodium, potassium, calcium, magnesium, and phosphorus. Thus, our kidneys are responsible for both the elimination of metabolic waste products from the blood and the maintenance of blood electrolyte and pH levels.
The kidney receives blood through the renal artery; this blood then passes through a structure of the kidney called a nephron (Figure 8.41). Filtration of the blood by the nephron occurs in three different processes in different locations: (1) glomerular filtration, in which fluid and low-molecular-weight molecules in the blood are filtered across the capillaries of the glomerulus and into the Bowman's capsule; (2) tubular reabsorption, the movement of substances from the renal tubule into the peritubular capillaries; and (3) tubular secretion, the movement of substances from the peritubular capillaries into the renal tubule.
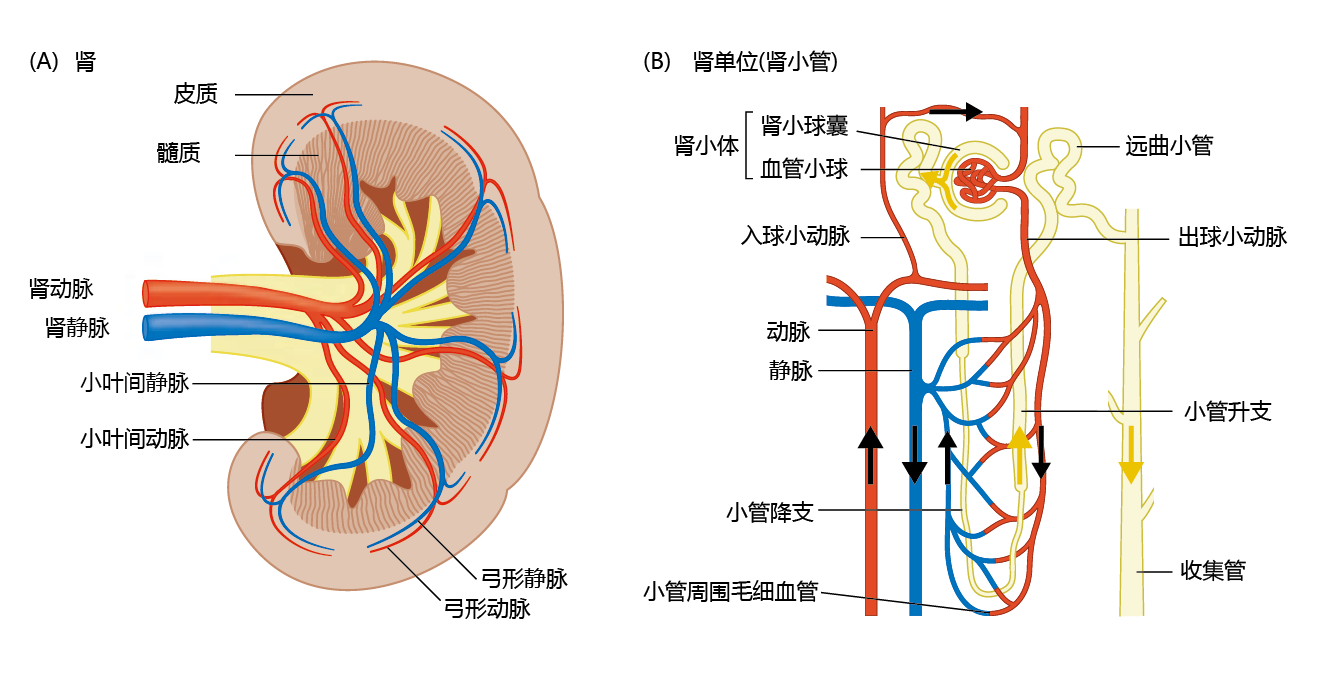
Figure 8.41 Anatomy of the kidney and nephron. (A) The gross structure of the kidney. (B) An individual nephron, showing the filtration system. Black arrows indicate the direction of blood flow through the arterioles, glomerulus, and peritubular capillaries. Yellow arrows indicate the direction of filtrate flow from Bowman's capsule to the collecting duct.
Glomerular filtration results from a pressure gradient between the glomerular capillaries and Bowman's capsule. Blood in the glomerular capillaries has a pressure of 60 mm Hg, whereas Bowman's capsule has a pressure of about 44 mm Hg. The greater pressure in the capillaries forces fluid and low-molecular-weight molecules out of the capillaries and into Bowman's capsule. The fluid in Bowman's capsule, called the glomerular filtrate, has the same concentration of substances as blood plasma.
Tubular reabsorption and secretion can occur by passive diffusion or mediated transport. Which process the nephron uses depends on the concentration of the substance in the renal tubule and in the peritubular capillaries. For example, the concentration of urea, a nitrogenous product of protein metabolism, in the glomerular filtrate is the same as that in the peritubular capillaries. As the glomerular filtrate moves through the tubule, water is reabsorbed and the concentration of urea in the filtrate decreases relative to that in the peritubular capillaries increases. As a result of this concentration gradient, urea passively diffuses from the glomerular filtrate into the peritubular capillaries. Nitrogen in the urea is thus returned to the circulation and is used to synthesize amino acids.
Mediated transport is used when a substance in the renal tubule or the peritubular capillaries must be transported against its concentration gradient, from lower to higher concentration. An example of mediated transport is the reabsorption of sodium through a membrane channel called the sodium/potassium ATP pump. Maintenance of proper cellular function requires keeping the intracellular concentration of sodium lower than that in the extracellular fluid. Conversely, the intracellular concentration of potassium must remain higher than the extracellular concentration. Thus, sodium passively diffuses from the lumen of the tubule into the epithelial cells lining the tubule. However, in tubular reabsorption, sodium passes from the tubular epithelial cells into the peritubular capillaries, against its concentration gradient. The sodium/potassium ATP pump allows sodium to move against its concentration gradient by exchanging sodium for potassium, using ATP as the energy source.
Kidneys help regulate blood pressure
Another important job of the kidney is to help the body maintain blood pressure by adjusting the amount of water in the blood. Moving water from the blood into the urine by tubular secretion decreases blood pressure. Tubular reabsorption maintains blood pressure by transferring water from the glomerular filtrate into the peritubular capillaries. The movement of water in the nephron is coupled to sodium reabsorption and is regulated by several hormones. Recall that sodium passively diffuses from the tubular lumen into the tubular epithelial cells. The removal of sodium lowers the osmolarity (i.e., raises the water concentration) of the glomerular filtrate, and water passively diffuses into the tubular epithelial cells—that is, water follows sodium. If the osmolarity of the peritubular capillaries is lower than that of the glomerular filtrate, water moves from the peritubular capillaries into the tubule. The coupling of water and sodium reabsorption explains the different colors of urine. If you do not drink enough water, the kidney reabsorbs water and the urine is yellow due to a high concentration of solutes. If you drink more water than your body needs, the kidney produces clear urine, because the concentration of solutes declines with the tubular secretion of water into the urine.
The amount of water reabsorbed by the kidney also depends on the permeability of the renal tubule. Tubular permeability is under physiological regulation by the hormone vasopressin, or antidiuretic hormone (ADH), secreted by the pituitary gland. When the hypothalamus (a region of the brain) senses a drop in blood volume, it sends a signal to the pituitary gland, which secretes ADH into the blood. ADH causes the opening of water channels (aquaporins) in the tubular epithelial cells, and the reabsorption of water increases. Conversely, an increase in blood volume inhibits the secretion of ADH, and more water remains in the tubule, resulting in a higher concentration of water in the urine.
Renal blood flow and kidney function decline with aging
Renal blood flow decreases with aging in terms of both total amount and percentage of cardiac output (the rate at which blood is pumped through the heart). The decrease in renal blood flow reflects a loss in the overall number of blood vessels in the kidney and the narrowing of the vessels. This loss of vessels occurs at all levels of the kidney, but the glomeruli seem to be the most affected. Beginning in a person's early thirties, the number of vessels in the glomerulus declines by about 10% per decade. Moreover, the remaining vessels are irregular and twisted, further limiting blood flow in the glomerulus.
Many of the arterial changes observed in the aging kidney are similar to those seen in other organs and include arteriolosclerosis and hypertrophy of the inner wall of the artery (see Chapter 9 for details on these conditions). One time-dependent change in the vasculature that seems to be more common in the kidney than in other organs is fibrointimal hyperplasia, abnormal growth in the intimal layer of the arterial wall. This condition is caused by the accumulation of plasma proteins in the vessel walls, a condition known as insudation, which causes vessel narrowing and reduced blood flow.
The time-dependent decline in the number and function of glomerular capillaries can also lead to a lower rate of fluid filtration from the glomerulus into the Bowman's capsule. The rate, or volume per unit of time, at which this fluid is filtered is known as the glomerular filtration rate (GFR). A young 60- to 70-kg person has a GFR of about 180 L/day. Given that total blood volume, on average, is about 6 L, the body's entire blood supply is filtered 60 times per day. Such a high volume of filtering allows the kidney to respond to and rapidly remove large quantities of metabolic waste products. The decrease in filtration due to aging is highly variable among individuals, ranging from 0% to about 20% of normal GFR. However, any change in the GFR will affect blood and body homeostasis.
The underlying cause of a reduced GFR is glomerulosclerosis, the degenerative scarring of the glomeruli. Some estimates have suggested that by age 80, 30%–40% of a person's glomeruli have stopped functioning due to this condition. Controversy exists as to whether glomerulosclerosis is a normal time-dependent event or is the result of high blood pressure. Time-dependent glomerulosclerosis cannot be distinguished from hypertension-related glomerulosclerosis in younger individuals. Furthermore, the condition is almost always found in older individuals with hypertension. Thus, it is not clear whether time-dependent glomerulosclerosis precedes or follows hypertension.


